Introduction to autoimmune disease and metal in medical and dental implants and devices
Medical and dental implants and devices containing metal have been associated with autoimmune disease.
Researchers have identified that autoimmune disease can be caused by a combination of
1) genetic components, and 2) metals (including those used in medical and dental implants and devices), pharmaceutical drugs, pollen, infectious agents, molds, and food allergies (such as gluten). There are now over 80 recognized autoimmune diseases, with some of the most common being diabetes, lupus, multiple sclerosis, rheumatoid arthritis, and celiac disease.
In the US, estimates of people afflicted by these debilitating health conditions range from 14.7 million to 50 million. It is important to note that the number of people suffering from autoimmune disease is increasing, and the use of medical and dental implants and devices containing metal is likewise increasing.
Autoimmune diseases associated with metal in medical and dental implants and devices
While numerous health conditions have been related to the presence of metals in the body, scientific research has clearly shown that autoimmune disease can be associated with metals used in dentistry and medicine, including metals in medical and dental implants, devices, and adjuvants (substances added to vaccines such as aluminum and mercury). Several of the autoimmune diseases studied for their relation to metal in medical and dental implants, devices, and adjuvants include the following:
| Amyotrophic Lateral Sclerosis (Lou Gehrig’s Disease) |
Autoimmune Thyroiditis | Chronic Fatigue Syndrome (Myalgic Encephalomyelitis / Chronic Fatigue Syndrome) |
| Crohn’s Disease | Diabetes (Type 1 Mellitis) | Fibromyalgia |
| Gulf War Syndrome | Lupus (Systemic Lupus Erythematosus) |
Macrophagic Myofasciitis |
| Multiple Sclerosis | Oral Lichen Planus | Rheumatoid Arthritis |
Sources of metal exposure from medical and dental implants and devices related to autoimmune disease
Some metals are recognized as essential to human life and serve important roles within the human body. However, the beneficial effects of trace elements are based on safe and adequate intake levels, with too little resulting in deficiencies and too much resulting in toxicities.
Other metals used as components in medical and dental implants, devices, and adjuvants have no established function in the human body. In addition to aluminum, which is both a neurotoxin and an immune stimulator, these include gold, mercury, nickel, palladium, platinum, silver, and titanium. Mercury is recognized as being toxic to humans even in low doses, and researchers have identified chromium, cobalt, copper, gallium, gold, iron, lead, manganese, mercury, nickel, platinum, silver, tin, vanadium, and zinc (among others) as metals of concern due to residential and occupational exposure.
Thus, medical and dental implants and devices placed directly into the human body merit significant consideration when evaluating the impact of metal exposure levels, especially in susceptible populations.
In some genetically susceptible individuals, metals can trigger allergies, and recent studies and reports tend to agree that metal allergies are on the rise. Clinical screening for metal allergy has been recommended, but the importance of patients reporting reactions to metals to their doctors has also been emphasized in the scientific literature.
In addition to reporting any rashes from jewelry, watches, or other metal exposures, it is essential for each patient to recognize the gamut of symptoms that can be related to the presence of a metallic medical or dental implant or device in their body, such as the development of an autoimmune disease. It is also vital for patients to remember that sensitization to metal can develop years after a medical or dental implant or device has been placed and that adverse effects can occur with or without the sign of a rash or eruption on the skin or in the mouth.
Removal of medical and dental implants and devices containing metal and potential recovery from autoimmune disease
Removal of medical and dental implants and devices that contain metal is an obvious course of action when adverse effects occur. Indeed, the scientific literature is abundant with studies and cases of individuals improving or recovering from autoimmune disease usually within a year or two after removal of the offending metal. In addition to metal-containing dental implants and devices, examples of materials containing metal removed include the copper IUD, nickel tubal ligation clips, and titanium screws and skull plates.
Some of health conditions that improved (or from which patients even recovered) after removal of metal medical and dental implants and devices include a variant of amyotrophic lateral sclerosis (Lou Gehrig’s Disease) known as progressive muscular atrophy, autoimmune thyroiditis, chronic fatigue syndrome, Crohn’s disease, fibromyalgia, multiple sclerosis, oral lichen planus, Sjögren’s syndrome, and systemic lupus erythematosus.
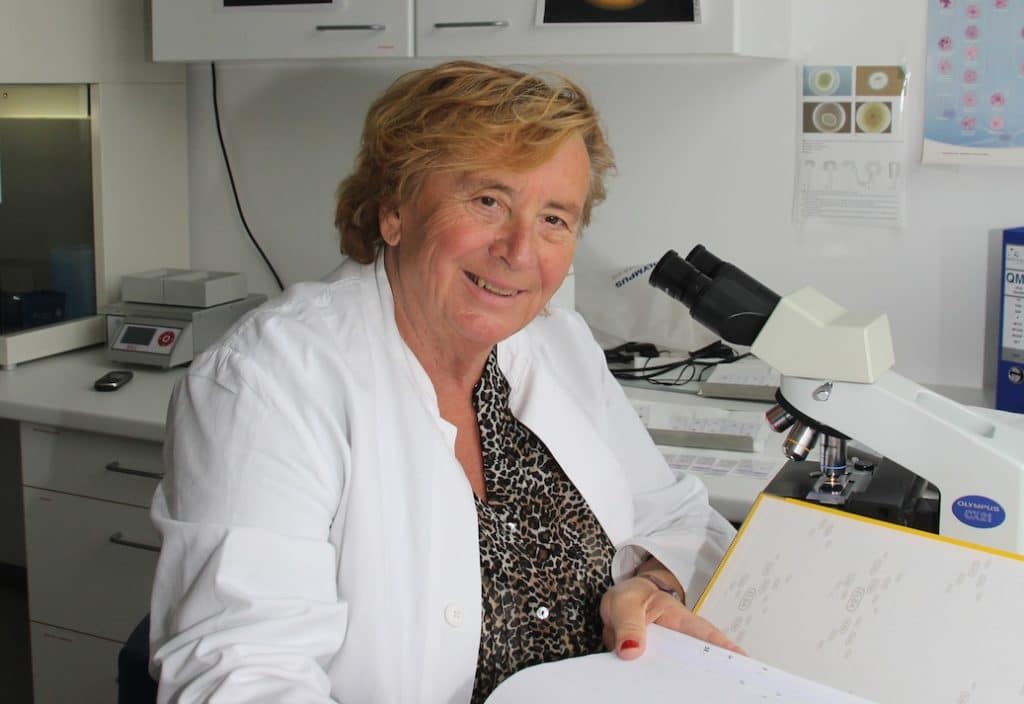
The late Vera Stejskal, PhD, studied the link between autoimmune disease and metals in medical and dental implants and devices. Her life’s work, which chronicled cases of recovery after safe removal of medical and dental implants and devices containing metal, is featured in this article.
In 1994, Dr. Vera Stejskal introduced the MELISA test, an alternative to patch testing for allergies designed to test for type IV delayed hypersensitivity to metals, including sensitivity to mercury. Much of Dr. Stejskal’s work involved using the testing to help diagnose patients with reactions to metals, thus facilitating the decision to have the medical and dental implants and devices containing metal safely removed and replaced with safer alternatives, and then, recording the health outcomes, the majority of which have involved significant improvement. Dr. Stejskal had a number of research articles published that included the science behind her work and the health improvements experienced by many of the patients.
In her research, Dr. Stejskal further warned about removing metal-containing medical and dental implants and devices safely. This is because an unsafe removal process of metal implants can cause serious injury (and even death) to the patient, in addition to the possibility of increased metal exposure.
Based on scientific research, the International Academy of Oral Medicine and Toxicology (IAOMT) has developed recommendations known as the Safe Mercury Amalgam Removal Technique (SMART) to assist in mitigating the potential negative outcomes of mercury exposure during amalgam removal. The IAOMT also offers education about alternatives to amalgam fillings so that patients can opt for a more “biocompatible” replacement, such as metal-free, ceramic options.
It is important to note that while many patients improve or even recover from autoimmune disease after the removal of a metal medical and dental implant or device, there are some who do not. One obvious reason for this is if the patient is still being exposed to the metal or a different sensitizer through another implant, device, adjuvant, or other source. Additional impediments in achieving improved health can include the presence of another illness and/or allergy, the need to eradicate Heliobacter pylori, exposure to certain pesticides, solvents, molds, and foods, hormonal imbalances, stress, smoking, a sedentary lifestyle, and countless other factors.
For all these reasons and more, it is imperative for patients battling autoimmune disease to work with their doctors and other healthcare professionals so that toxins and allergens such as metal medical and dental implants and devices are kept out of their bodies and healthier, safer options are put in to replace them.
For more information about the research of Dr. Vera Stejskal